 |
A woman in her 50s with history of hematopoietic stem cell transplantation presenting with headache, chest pain and fevers |
- History of Present Illness
- A woman in her 50s presented with headache, chills, lack of appetite and self-described “flu like symptoms”. Her symptoms started 6 days prior to presentation with dyspnea and right sided pleuritic chest pain. She was seen at an urgent care where a chest x-ray was suggestive of pneumonia. The patient was prescribed azithromycin and cefpodoxime, without improvement. She then developed a fever to 101.9F with shortness of breath prompting presentation to the emergency room.
- Past Medical History
- Acute myeloid leukemia status post allogeneic matched unrelated donor hematopoietic stem cell transplantation (Cytomegalovirus donor negative, recipient positive) two years prior
- Aplastic anemia status post 5 cycles of cyclosporine and antithymocyte globulin completed 8 months prior
- Hypogammaglobulinemia receiving monthly intravenous immunoglobulin therapy
- Medications
- Atovaquone 1500mg suspension by mouth daily
- Valacyclovir 500mg tablet by mouth daily
- Posaconazole 300mg tablet by mouth daily
- Cyclosporine 60mg solution by mouth 2 times daily
- Eltrombopag 125mg tablet by mouth daily
- Deferasirox 360mg tablet by mouth daily
- Prednisone 4mg tablet by mouth daily
- Allergies
- Penicillin (rash)
- Epidemiological History
- Patient lives with her husband in the Midwest region of the United States. No recent travel outside of the Midwest. She has cats. Her husband cleans their litter box. She works at a school. Occasionally drinks alcohol, no recreational drug use, no tobacco use.
- Physical Examination
- Patient appeared comfortable. The blood pressure was 113/73, respiratory rate of 22 breaths per minute, pulse 84 beats per minute, temperature 101.9F, saturating 93% SpO2 on room air. There were crackles in the right mid-lung and egophony. Scattered age indeterminate ecchymoses on bilateral upper extremities. The exam was otherwise normal.
- Studies
White blood cell count of 25,000/uL (reference range 3.5-10.5 103/uL) with a neutrophil predominance, hemoglobin 8.4 (reference range 11.6-15.4 g/dL), platelets 20,000/uL (reference range 140-390 103/uL), potassium 2.6 mmol/L (reference range 3.5-5.1 mmol/L), creatinine 1.19 mg/dL (reference range 0.60-1.30 mg/dL), d-dimer 1931 ng/mL D-DU (reference range < =230 ng/mL). Respiratory viral panel was negative, SARS-CoV2 antigen testing was negative, urine Legionella antigen was negative, urine Streptococcus pneumoniae antigen was negative, blood and urine cultures negative. Posaconazole level 3.6. Patient was unable to provide a sputum sample.
A chest radiography (posterior-anterior and lateral) demonstrated a right upper lobe pneumonia (Figure 1). Computed tomography (CT) of the chest (Figure 2) with contrast demonstrated a mass like consolidative opacity within the right upper lobe containing small foci of gas, concerning for pulmonary abscess. Scattered subcentimeter pulmonary nodules, some are stable but the majority are new.
 - Figure 1: Chest radiography posterior-anterior and lateral.

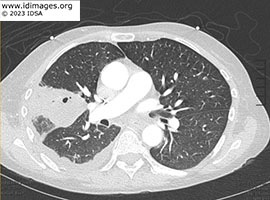 - Figure 2: Computed tomography scan of chest with contrast.

- Clinical Course Prior to Diagnosis
The patient suffered a fall and underwent head CT scan which demonstrated abnormalities. A subsequent MRI of the brain demonstrated numerous small ring-enhancing lesions throughout both cerebral hemispheres (Figure 3). A bronchoscopy with BAL demonstrated 97 cells, 71% neutrophils, aerobic, anaerobic, fungal, AFB, Legionella cultures, Pneumocystis jirovecii PCR and cytology were all negative. No biopsy was performed. Cell free DNA sequencing of plasma (Karius TestTM) was sent. Patient expressed preference to complete workup as an outpatient when a nodule was felt on her right calf. A new area of pain and swelling had emerged which on vascular ultrasound appeared to be an abscess. An MRI of the tibia/fibula demonstrated a 1.5x1.4cm peripherally enhancing lesion in the medial gastrocnemius muscle concerning for intramuscular abscess (figure 4). Interventional radiology performed aspiration of the abscess.
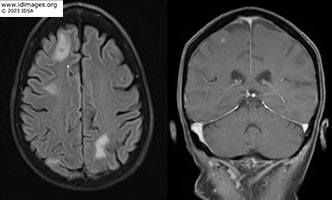 - Figure 3: MRI brain with and without contrast.

 - Figure 4: MRI right tibia/fibula

- Diagnostic Procedure(s) and Result(s)
Noninvasive serological testing as follows: Toxoplasma IgG, IgM negative, Cryptococcus antigen negative, Histoplasma antigen negative, (1-3)-beta-D-Glucan assay negative, Blastomyces antigen negative, Quantiferon TB Gold indeterminate due to inadequate mitogen response.
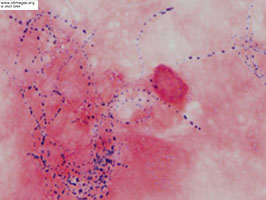
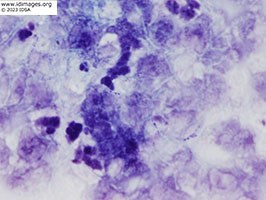
The right calf abscess fluid demonstrated beaded branching gram positive rods on gram stain (Figure 5). Kinyoun stain of leg aspiration demonstrated weakly acid-fast rods (Figure 6). Cultures were notable at 48 hours for chalk white colonies on buffered charcoal yeast abstract (BCYE) (Figure 7) and gram stain revealed branching gram-positive rods. Sanger sequencing of the 16S ribosomal rRNA gene revealed 99% similarity to Nocardia arthritidis. Cell free DNA sequencing of plasma (Karius TestTM) also yielded Nocardia but was unable to distinguish between the following species: Nocardia exalbida, Nocardia gamkensis, Nocardia arthritidis.
 - Figure 5: Gram stain of right calf abscess fluid - beaded branching gram positive rods.

 - Figure 6: Kinyoun stain of right calf abscess fluid - demonstrates weakly acid-fast rods.

 - Figure 7: Buffered charcoal yeast extract (BCYE) agar plate of right calf abscess fluid.

- Treatment and Followup
Patient treated with ceftriaxone IV 2gm every 12 hours for 3 months and sulfamethoxazole-trimethoprim 800-160mg 1.5mg tablets by mouth every 12 hours for plan of at least 12 months of therapy. Repeat CT chest 1 month (Figure 8a) and 6 months (Figure 8b) after start of antimicrobial therapy showed marked improvement in the cavitary consolidation in the right upper lobe. MRI brain after 6 months of treatment with near complete resolution of prior infection (Figure 9b).
 - Figure 8A: Computed tomography scan of chest after 1 month of treatment

 - Figure 8B: Computed tomography scan of chest after 6 months of treatment

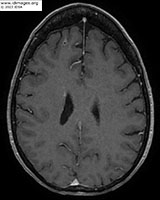 - Figure 9: MRI brain after 6 months of treatment.

- Discussion
Nocardia species are aerobic gram-positive and partly acid-fast bacteria that are a normal part of the soil microflora, salt, and fresh-water aquatic environments. Nocardia is found in common sources such as tap water, house dust, and beach sands [1]. Given the ubiquitous nature of the bacteria, infections are mostly noted in immunocompromised hosts however approximately one-third of infections occur in immunocompetent individuals. Although the mechanism of pathogenicity is not entirely understood, it is believed that Nocardial species can evade or neutralize the microbicidal activities of the host [2]. Infections are typically insidious with onset of symptoms coursing over weeks. Sites of infection can be localized to point of entry or the organism can disseminate to other organs via the bloodstream and form abscesses in the brain, skin, and lung as well as other sites For this reason, it is important to evaluate for disseminated disease with brain and lung imaging [3]. Nocardial colonization is uncommon so when the bacteria are identified, it is usually considered pathogenic [4]. Diagnosis involves microbiologic identification from suspected sites of infection. However, laboratory personnel should be notified that Nocardia is suspected as it can be difficult to culture and requires special growth media (BCYE) and longer incubation period [5]. Molecular tests, such as polymerase chain reaction (PCR) or whole genome sequencing are also methods utilized in identifying the pathogen. Treatment is guided by antimicrobial susceptibility testing although most isolates are susceptible to trimethoprim-sulfamethoxazole (TMP-SMX) [6]. Susceptibility patterns vary between Nocardia species and as such, empiric coverage with two or three agents is preferred practice in patients with severe infection. Duration of treatment varies depending on extent of disease and underlying host factors, ranging from 3 to 12 months, and in some cases followed by lifelong suppressive therapy.
Although cutaneous Nocardia lesions comprise 5-22% of all Nocardiosis cases, Nocardia as a cause of muscle abscess is a rare complication. The likely mechanism is hematogenous spread from a pulmonary lesion. There are nine case reports of muscle abscesses due to Nocardia species, one in an immunocompetent cattle inspector due to Nocardia farcinica, with no direct trauma [7].
In establishing a diagnosis, the non-invasive serological testing and bronchoscopy with BAL were all negative. Sputum or BAL samples can be adequate for diagnosing pulmonary Nocardial infection. In one observational study, expectorated sputum was diagnostic in 45 of 51 individuals who had pulmonary Nocardial infection [8]. A pulmonary biopsy was suggested in this case, but patient did not wish to pursue this. The diagnosis was established due to the presence of a fluctuant mass in the patient’s right calf which subsequently underwent biopsy and culture. This specimen yielded Nocardia arthritidis, identified by 16S ribosomal rRNA sequencing. Prior to knowledge of the calf abscess, cell free DNA sequencing of plasma (Karius TestTM) was performed. The infection had clinically metastasized to various parts of the body and there were fragments of non-encapsulated microbial DNA in the plasma at significant levels, which were detected by the Karius TestTM, however, this type of testing was not able to differentiate between Nocardia exalbida, Nocardia gamkensis, Nocardia arthritidis.
- Final Diagnosis
- Disseminated Nocardia arthritidis with pulmonary, brain, and muscle involvement.
- References
-
- Lederman ER, Crum NF. A case series and focused review of nocardiosis: clinical and microbiologic aspects. Medicine (Baltimore). 2004 Sep;83(5):300-313. doi: 10.1097/01.md.0000141100.30871.39. PMID: 15342974.
PMID:15342974 (PubMed abstract)
- Beaman BL, Beaman L. Nocardia species: host-parasite relationships. Clin Microbiol Rev. 1994 Apr;7(2):213-64. doi: 10.1128/CMR.7.2.213. PMID: 8055469; PMCID: PMC358319.
PMID:8055469 (PubMed abstract)
- Martínez-Barricarte R. Isolated Nocardiosis, an Unrecognized Primary Immunodeficiency? Front Immunol. 2020 Oct 20;11:590239. doi: 10.3389/fimmu.2020.590239. PMID: 33193422; PMCID: PMC7606290.
PMID:33193422 (PubMed abstract)
- Margalit I, Muhsen K, Ben Ari Y, Ben-Zvi H, Shostak Y, Krause I, Goldberg E. Nocardia colonization in contrast to nocardiosis: a comparison of patients' clinical characteristics. Eur J Clin Microbiol Infect Dis. 2020 Apr;39(4):759-763. doi: 10.1007/s10096-019-03796-5. Epub 2019 Dec 20. PMID: 31863237.
PMID:31863237 (PubMed abstract)
- McNeil MM, Brown JM. The medically important aerobic actinomycetes: epidemiology and microbiology. Clin Microbiol Rev. 1994 Jul;7(3):357-417. doi: 10.1128/CMR.7.3.357. PMID: 7923055; PMCID: PMC358331.
PMID:7923055 (PubMed abstract)
- Brown-Elliott BA, Biehle J, Conville PS, Cohen S, Saubolle M, Sussland D, Wengenack N, Kriel K, Bridge L, McNulty S, Vasireddy R, Wallace RJ Jr. Sulfonamide resistance in isolates of Nocardia spp. from a US multicenter survey. J Clin Microbiol. 2012 Mar;50(3):670-2. doi: 10.1128/JCM.06243-11. Epub 2011 Dec 14. PMID: 22170936; PMCID: PMC3295118.
PMID:22170936 (PubMed abstract)
- Ukai Y, Fujimoto N, et al. Case of muscle abscess due to disseminated nocardiosis in a patient with autoimmune hemolytic anemia, and review of the published work. J Dermatol. 2012 May;39(5):466-9. doi: 10.1111/j.1346-8138.2011.01393.x. PMID: 22011194.
PMID:22011194 (PubMed abstract)
- Saubolle MA, Sussland D. Nocardiosis: review of clinical and laboratory experience. J Clin Microbiol. 2003 Oct;41(10):4497-501. doi: 10.1128/JCM.41.10.4497-4501.2003. PMID: 14532173; PMCID: PMC254378.
PMID:14532173 (PubMed abstract)
- Notes
ID Week 2023 - Fellows' Day
Tirajeh Saadatzadeh, MD, Northwestern University - Citation
- If you refer to this case in a publication, presentation, or teaching resource, we recommend you use the following citation, in addition to citing all specific contributors noted in the case:
Case #23007: A woman in her 50s with history of hematopoietic stem cell transplantation presenting with headache, chest pain and fevers [Internet]. Partners Infectious Disease Images. Available from: http://www.idimages.org/idreview/case/caseid=611
- Other Resources
-
Healthcare professionals are advised to seek other sources of medical information in addition to this site when making individual patient care decisions, as this site is unable to provide information which can fully address the medical issues of all individuals.
|
|