 |
Elderly female with fever and epigastric pain |
- History of Present Illness
A female in her seventies presented to the emergency department with one day of fever and chills associated with myalgia and epigastric pain. She was hospitalized the week before for work-up of myelodysplastic syndrome requiring a bone marrow biopsy. Blood cultures done on this admission were positive for gram-positive rods in three out of four bottles (Figure 1-2) for which infectious disease was consulted.
She reported epigastric pain with no radiation or association with food. She denied having dysphagia or odynophagia. She denied pain at the site of the bone marrow biopsy. There was no recent trauma and no known skin infections. She has a history of fishbone stuck in her esophagus requiring surgical removal seven years ago.
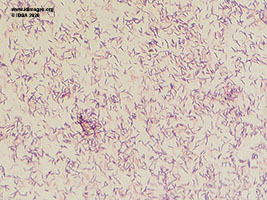 - Figure 1. Gram stain, Blood: 100x Oil immersion: predominantly gram-positive rods, non-spore forming.

 - Figure 2. Blood Culture showing small grey alpha hemolytic colonies at 48 hours.

- Past Medical History
- Diabetes, Hypertension
- Epidemiological History
Immigrated to the U.S.A from China more than 10 years ago. Lives alone, no pets, no recent travel. Patient does not eat raw food; reported eating fish daily. Patient denied consumption of unpasteurized dairy or probiotic use.
- Physical Examination
At the time of consult, the patient had a temperature of 97.7F (36.5C), blood pressure of 142/75 mm Hg, pulse 80 beats per minute, and respiration rate of 18 breaths per minute with a saturation of 100% on room air. She appeared uncomfortable. No skin or mucosal lesions. Tender epigastric region without rebounding or guarding. Tender lumbar spine, which was reported to be chronic. The rest of the exam was normal.
- Studies
Laboratory investigations were significant for white blood cell count of 14.8 k/ul (range 4-11 k/ul) with hemoglobin of 8.8 g/dl (range 11-15 g/dl), which was her baseline. C-reactive protein was 102.60 mg/dl (range 0-7.48 mg/dl). Electrolytes, kidney function, and liver function tests were normal. Urinalysis showed no pyuria, and urine culture was negative. Blood cultures from admission showed gram-positive rods in three out of four bottles (Figure 1-2). Subsequent blood cultures, drawn a day after, were negative. Chest X-ray (CXR) showed no infiltrate (Figure 3).
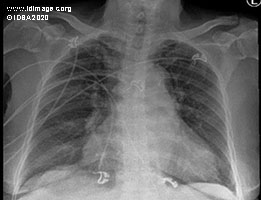 - Figure 3. Chest X-Ray (CXR) on admission.

- Clinical Course Prior to Diagnosis
The patient remained afebrile with hemodynamic stability; examination remained stable, with no evidence of heart failure. Blood cultures flagged for an organism on our matrix-assisted laser desorption ionization time-of-flight (MALDI-TOF) mass spectrometry on day six of admission. VITEK -2 flagged positive for the same organism on day eight of admission. The organism was oxidase-negative, catalase-negative, non-motile, non-spore-forming, and alpha-hemolytic on blood agar. The blood culture plate was sent out for confirmation, as these machines at our hospital have not been validated for identification for this organism. While awaiting confirmation, the patient was kept on antibiotics, and a transthoracic echocardiogram (TTE) was obtained.
- Diagnostic Procedure(s) and Result(s)
The blood culture came back as Erysipelothrix rhusiopathiae. TTE showed multiple large vegetations on the tricuspid valve with possible small vegetation on the aortic valve. This finding was confirmed with a trans-esophageal echocardiogram (TEE), which showed thickened tricuspid leaflets with multiple large mobile tricuspid valve vegetations, moderate to severe tricuspid regurgitation (Figure 4). Moderately thickened aortic valve. Small mobile echo-density 0.5 cm in length on the ventricular surface of the aortic valve, likely a vegetation (Figure 5). Moderate aortic regurgitation. No vegetation on the mitral or pulmonic valve seen.
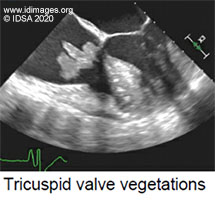 - Figure 4. Transesophageal Echocardiogram image of vegetation on Tricuspid Valve.

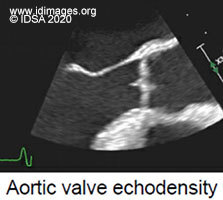 - Figure 5. Transesophageal Echocardiogram image of vegetation on Aortic Valve.

- Treatment and Followup
On further questioning, she reported daily consumption of unsold fish from the market. She mentioned having cooked it well with no injuries on the skin while preparing food; however, she stated she might have missed removing the smaller bones while preparing the fish. She did not remember any fishbone being stuck in her throat. Also, on examination, we did not find any skin lesions, but she did complain of epigastric pain on admission, which could have been due to an injury from the fishbone. We obtained chest imaging which did not show any signs of esophageal perforation.
The patient was initially on intravenous vancomycin and ampicillin/sulbactam while awaiting the culture results. She was then switched to intravenous penicillin G once confirmation of the organism was obtained. The patient remained hemodynamically stable with no respiratory or neurological symptoms. She was seen by cardiothoracic surgery after her echocardiography results and was planned for surgery.
She underwent aortic and tricuspid valve replacement. In the operating room, it was noted that she had multilobulated vegetations involving all three leaflets of the tricuspid valve. Also, the chordae tendineae and papillary muscles contained vegetations. The inspection of the aortic valve demonstrated that each of the three leaflets had vegetations on the ventricular side. Pathology of the valves showed acute endocarditis on the aortic valve and acute fibrinous endocarditis with bacterial colonies on the tricuspid valve. Gram stain showed gram-positive colonies.
The patient was discharged on penicillin. She had subsequent imaging of her chest, which showed emboli to lungs likely septic in origin, raising suspicion for repeat endocarditis on the newly placed tricuspid valve. She underwent repeat TEE and was ruled out for endocarditis. The patient completed six weeks of intravenous penicillin. She is being followed in the infectious disease clinic and is recovering well at five months after her initial presentation.
- Discussion
Erysipelothrix rhusiopathiae is a catalase-negative, indole-negative, non-motile, non-spore-forming, facultative anaerobic gram-positive bacillus. It is commonly alpha-hemolytic on blood agar and may be misidentified as a viridans streptococcus (1). Erysipelothrix and Bacillus species may be differentiated by the absence and presence of spores, respectively. Unlike other gram-positive non-sporulating rods (Lactobacillus species, Listeria monocytogenes, Arcanobacterium species), Erysipelothrix rhusiopathiae produces hydrogen sulfide on triple sugar iron media (2). Moreover, Listeria and Arcanobacterium species are beta-hemolytic. Listeria also is a catalase-positive and motile organism.
Erysipelosthrix rhusiopathiae is ubiquitous in nature and has been reported to be a colonizer of swine, fish, shellfish, birds, and even insects, with the pig being the main reservoir (1). In humans, it is primarily associated with occupational exposure - butchers, slaughterhouse workers, farmers, and fish handlers have the highest risk of acquiring the infection (2). Infections following the ingestion of contaminated frozen fish and pork have also been documented (3). People with cirrhosis, alcohol use disorder, poorly controlled diabetes are at higher risk.
There are three well defined clinical categories of human disease. The most common form of infection is a localized cutaneous form called erysipeloid, which occurs as a result of direct inoculation with the infected animal or fish. The second form is rare, a diffuse cutaneous eruption with systemic symptoms. The third form is a systemic infection, predominately bacteremia, often associated with endocarditis (4). It is noteworthy that previously, bacteremic infection, with or without endocarditis, was considered most commonly a primary infection rather than dissemination from localized cutaneous lesions (1). Recent literature shows an increasing rate of bacteremia starting from localized cutaneous lesions (3).
E. rhusiopathiae infection may occur more commonly than reports suggest. It is likely underdiagnosed and under-reported because of the resemblance it bears to other infections and the problems that may be encountered in isolation and identification of this pathogen. Furthermore, gram-positive rods cultured from the blood are often dismissed as diphtheroids and not fully identified.
The definitive diagnosis of infection with E. rhusiopathiae requires isolation of the organism from a biopsy specimen, blood, or other sterile body fluid. Standard methods for culturing blood or biopsy tissue should suffice if incubation is continued up to 7 days (4). It is noteworthy that MALDI-TOF has been shown to accurately and rapidly identify Erysipelothrix rhusiopathiae (5).
Erysipelothrix rhusiopathiae is different from other bacteria, as it tends to affect normal native heart valves with peculiar tropism seen for aortic valve (1). E. rhusiopathiae is exquisitely susceptible to penicillin and carbapenems but has intrinsic resistance to vancomycin. Even with the administration of appropriate drugs, 36% of patients need valve replacement due to significant valve destruction. The complications, such as mycotic aneurysm, valve perforation, and myocardial abscess, are the same among patients with E. rhusiopathiae as other organisms, but the mortality rate is much higher (38% versus 20%) (1). Intrinsic resistance to vancomycin could be contributing to higher mortality seen with E. rhusiopathiae, as vancomycin is often the first choice for empiric coverage of gram-positive rod bacteremia. Treatment for endocarditis is typically intravenous penicillin for four to six weeks.
Our case demonstrates Erysipelothrix rhusiopathiae bacteremia with aortic and tricuspid valve endocarditis without any evidence of skin lesions. We postulate that she had bacteremia after ingestion of contaminated fish followed by gastrointestinal colonization, which allowed the organism to gain access to the patient’s circulation. The purpose of this case report is to emphasize the subtle microbiological differences between different gram-positive rods and the importance of full workup of gram-positive rod bacteremia and not dismissing them as contaminants. Providers should think about Erysipelothrix rhusiopathiae in the right setting i.e., patients with high-risk exposures and risk factors; potential of having bacteremia in the absence of skin findings, and associated endocarditis even in the absence of murmur. It is important to note that this organism causes significant valve destruction of native valves, thereby increasing the need for valve replacement. E. rhusiopathiae has intrinsic resistance to vancomycin, and infection with this organism has been associated with a higher mortality rate.
- Final Diagnosis
Erysipelothrix rhusiopathiae bacteremia with native aortic and tricuspid valve endocarditis
- References
-
- Gorby GL, Peacock JE Jr. Erysipelothrix rhusiopathiae endocarditis: microbiologic, epidemiologic, and clinical features of an occupational disease. Rev Infect Dis. 1988;10(2):317-325.
PMID:3287562 (PubMed abstract)
- Venditti M, Gelfusa V, Castelli F, Brandimarte C, Serra P. Erysipelothrix rhusiopathiae endocarditis. Eur J Clin Microbiol Infect Dis. 1990;9(1):50-52.
PMID:2137414 (PubMed abstract)
- Kichloo AA, Hallac A, Mousavi B, Hirekhan O. Nonspecific Erysipelothrix rhusiopathiae Bacteremia in a Patient with Subclinical Alcoholic Liver Disease. Case Rep Infect Dis. 2013; 2013:474593.
PMID:23819078 (PubMed abstract)
- Mandell G, Douglas R, Bennett J, Dolin R, Blaser M. Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, Pa: Elsevier, Saunders; Ninth edition. Page 209, 2575-2577.e1
- Farfour E, Leto J, Barritault M, et al. Evaluation of the Andromas matrix-assisted laser desorption ionization-time of flight mass spectrometry system for identification of aerobically growing Gram-positive bacilli. J Clin Microbiol. 2012;50(8):2702-2707.
PMID:22692743 (PubMed abstract)
- Notes
ID week Fellows' Day 2020 - oral presentation
This case was contributed by:
Shrein Saini, MD, David R. Stone, MD
Tufts Medical Center, Boston, MA
The case was originally presented at ID Week 2020, a joint effort of Infectious Diseases Society of America (IDSA), HIV Medical Association, Pediatric Infectious Diseases Society (PIDS), and the Society for Healthcare Epidemiology of America (SHEA), during an interactive session on Fellows' Day. Copyright Infectious Disease Society of America (IDSA), 2019. Used with permission.
- Citation
- If you refer to this case in a publication, presentation, or teaching resource, we recommend you use the following citation, in addition to citing all specific contributors noted in the case:
Case #20005: Elderly female with fever and epigastric pain [Internet]. Partners Infectious Disease Images. Available from: http://www.idimages.org/idreview/case/caseid=587
- Other Resources
-
Healthcare professionals are advised to seek other sources of medical information in addition to this site when making individual patient care decisions, as this site is unable to provide information which can fully address the medical issues of all individuals.
|
|