 |
Sporotrichoid Rash in an Immunocompromised Patient |
- History of Present Illness
A man in his fifties with end-stage renal disease status post living related renal transplant about 2 years before admission (complicated by graft rejection) presented with a 3-week history of a linear nodular skin rash over his left lower extremity. He reported developing a nodule and erythema over the medial aspect of his left shin after performing yard work that included cleaning a stack of old decaying wood. He did not recall any physical contact with the wood at the time of his yard work, but reported a mechanical fall when he sustained a small wound over the left distal anterior shin that had healed. His physician prescribed a 7-day course of cephalexin one week later for suspected cellulitis. He did not respond to antibiotics, but instead developed new skin nodules distally and proximally in a sporotrichoid pattern over the next few weeks. Some of his lesions broke down and started to drain a yellowish fluid. He denied any fevers, chills, cough, chest pain, shortness of breath, or abdominal symptoms.
- Medications
- Mycophenolate 500 mg twice daily, Tacrolimus 6 mg twice daily, Prednisone 5 mg daily
- Epidemiological History
- The patient lived in the northeast US with no recent travel, or animal exposures.
- Physical Examination
The patient’s vital signs were normal at the outpatient clinic visit: Temperature 97.3ºF (36.3ºC), blood pressure 150/82 mm Hg, pulse 85 beats per minute, respirations 16 breaths per minute, and an oxygen saturation of 98% on room air. He was well-appearing and in no acute distress. The exam was notable for multiple nodules of approximately 1-2 cm in diameter distributed in a string-like pattern along medial aspect of LLE associated with some ulcerations, a small amount of purulent discharge, tenderness, and mild erythema as well as hyperpigmentation (Figure 1A). The rest of his exam was within normal limits.
 - Figure 1A. Image of the patient’s leg demonstrating skin lesions with sporotrichoid pattern before treatment with voriconazole.

- Studies
- The complete blood count revealed a white blood cell count of 1.6 per microliter of blood (reference range 3.4-11.2) and an absolute neutrophil count of 0.9 per microliter of blood (reference range 1.8-7.0), hemoglobin of 9.1 grams per deciliter (reference range 13.3-17.7), and normal platelets. His serum creatinine was 3.51 milligram per deciliter (reference range 0.64-1.27), and his electrolytes and liver function tests were otherwise normal. Blood cultures were negative.
A magnetic resonance imaging (MRI) of the left lower leg demonstrated circumferential subcutaneous edema but otherwise no discrete abscesses, osteomyelitis, or other abnormal findings.
- Clinical Course Prior to Diagnosis
- After his symptoms progressed, he presented to the emergency room where clindamycin was started and Dermatology consulted. A punch biopsy was obtained and sent for histopathology and culture (Figure 2). He was then discharged with a 10-day course of Linezolid and referred for outpatient Infectious Diseases consultation.
- Diagnostic Procedure(s) and Result(s)
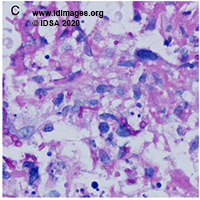
Tissue obtained from a skin punch biopsy showed a necrotizing neutrophilic and granulomatous inflammatory reaction associated with a fungus that appeared as irregular septated hyphae and yeast forms (Figure 2). Fungal wound cultures eventually grew Scedosporium apiospermum.
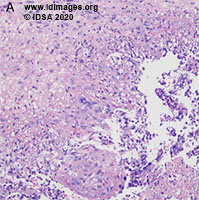 - Figure 2A. Representative histopathology from the skin biopsy. Hematoxylin and eosin staining demonstrates a focus of necrotizing neutrophilic and granulomatous inflammation at the base of the biopsy (20x magnification)

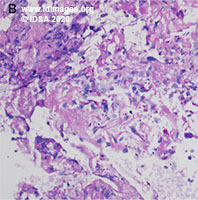 - Figure 2B. Representative histopathology from the skin biopsy. A fungus is discernible on periodic acid-Schiff (PAS) stain (40x magnification)

 - Figure 2C. Representative histopathology from the skin biopsy showing PAS stain at 100x magnification

 - Figure 2D. Representative histopathology from the skin biopsy. Grocott Methenamine Silver (GMS) stain with the fungus appearing as irregular septated hyphae and yeast forms (100x magnification)

- Treatment and Followup
The patient was initially treated with itraconazole for suspected sporotrichosis prior to the result of his cultures. With identification of Scedosporium apiospermum on fungal wound cultures, itraconazole was changed to voriconazole. His neutrophils gradually recovered and he was no longer neutropenic. The doses of his immunosuppressants were not changed. He was treated of a total of 7-8 months with voriconazole. At his 7-month follow-up, his skin lesions had markedly improved (Figure 1B).
 - Figure 1A. Image of the patient’s leg demonstrating skin lesions with sporotrichoid pattern before treatment with voriconazole.

 - Figure 1B. Image of the patient’s leg with resolved skin lesions after treatment with voriconazole.

- Discussion
Scedosporium species are ubiquitous environmental fungi found in the soil and polluted waters worldwide [1]. The two clinically important species in the genus are Scedosporium apiospermum and Scedosporium prolificans [2]. These species are considered emerging opportunistic pathogens, capable of causing local and invasive diseases in humans which range from cutaneous and subcutaneous tissue infections to disseminated infections in immunocompromised hosts [2]. Other sites of infections include the central nervous system, eyes, sinuses, lungs, abdomen, blood, and other locations [2]. Infection can occur through inhalation of spores or traumatic inoculation of the fungus [2]. In patients who present with skin infections, scedosporiosis can manifest with a sporotrichoid rash. The increasing incidence of Scedosporium infections is thought to be related to the increased use of immunosuppressive agents, such as antineoplastics and corticosteroids, and antifungal agents in the immunocompromised host that have activity against Candida and Aspergillus species but limited or no activity against Scedosporium [2,3]. Diagnosis of Scedosporium species is typically made by detecting the fungus from clinical specimens through direct microscopic examination or histological analysis and by culture on the appropriate media [3]. This could be challenging as it may be difficult to distinguish Scedosporium species from species of Aspergillus or Fusarium, as they may all present with dichotomous branching, hyaline hyphae, and regular hyphal septation [3, 4]. New approaches of diagnostics with non-culture-based molecular methods, such as mass spectroscopy and nucleic acid sequencing, are being pursued to improve the diagnosis of this fungal disease [3]. Treatment of Scedosporium infections could also be challenging because of its intrinsic resistance and reduced susceptibility to some of the commonly used antifungal agents. Scedosporium species are typically resistant to polyenes and the triazole fluconazole. They also demonstrate reduced susceptibility to echinocandins, such as micafungin [3,5]. Most guidelines recommend voriconazole as first-line therapy [3]. While not United States Food and Drug Administration-approved, isavuconazole has shown good in vitro activity, though clinical experience is limited [3,6]. In patients with invasive disease, combination therapy with several antifungal agents and reversal of immunosuppression are often considered [3, 7]. In our case, the patient had a localized skin and soft tissue infection with Scedosporium that was successfully managed with voriconazole. However, given his initial neutropenia which later recovered, it should be acknowledged that the recovery of the neutrophils may have been as important as the antifungal medication to this patient’s healing process. Given the increasing incidence of Scedosporium and other invasive fungal infections in the immunocompromised population along with the intrinsic antimicrobial resistance of Scedosporium species, we suggest clinicians consider obtaining clinical specimens through a tissue biopsy, when available, for routine cultures and pathologic analysis when treating an immunocompromised patient who has failed prior antibiotic therapy for a persistent rash. We also recommend that Scedoporium species be considered in the differential diagnosis of a sporotrichoid rash.
- Final Diagnosis
Scedosporium skin and soft tissue infection in an immunocompromised patient.
- References
-
- Johnson LS, Shields RK, Clancy CJ. Epidemiology, clinical manifestations, and outcomes of scedosporium infections among solid organ transplant recipients. Transpl Infect Dis. Published online 2014.
PMID:24962102 (PubMed abstract)
- Cortez KJ, Roilides E, Quiroz-Telles F, et al. Infections caused by Scedosporium spp. Clin Microbiol Rev. Published online 2008.
PMID:18202441 (PubMed abstract)
- McCarthy MW, Katragkou A, Iosifidis E, Roilides E, Walsh TJ. Recent advances in the treatment of scedosporiosis and fusariosis. J Fungi. Published online 2018.
PMID:29912161 (PubMed abstract)
- Salehi E., Hedayati M.T., Zoll J., Rafati H., Ghasemi M., Doroudinia A., Abastabar M., Tolooe A., Snelders E., van der Lee H.A., et al. Discrimination of aspergillosis, mucormycosis, fusariosis and scedosporiosis in formalin-fixed paraffin-embedded tissue specimens using multiple real-time quantitative PCR assays. J. Clin. Microbiol. 2016.
PMID:27605714 (PubMed abstract)
- Lackner M., Hagen F., Meis J.F., Gerrits van den Ende A.H., Vu D., Robert V., Fritz J., Moussa T.A., de Hoog G.S. Susceptibility and diversity in the therapy-refractory genus Scedosporium. Antimicrob. Agents Chemother. 2014;58:5877–5885.
PMID:25070092 (PubMed abstract)
- Pfaller M.A., Messer S.A., Rhomberg P.R., Jones R.N., Castanheira M. In vitro activities of isavuconazole and comparator antifungal agents tested against a global collection of opportunistic yeasts and molds. J. Clin. Microbiol. 2013;51:2608–2616.
PMID:23740727 (PubMed abstract)
- McCarthy M., Rosengart A., Schuetz A.N., Kontoyiannis D.P., Walsh T.J. Mold infections of the central nervous system. N. Engl. J. Med. 2014;371:150–160.
PMID:25006721 (PubMed abstract)
- Notes
ID week Fellows' Day 2020 - oral presentation
This case was contributed by:
Khanh Pham, MD, Cynthia Magro, MD, Markus Plate, MD
New York Presbyterian/Weill Cornell Medical Center, New York, NY
The case was originally presented at ID Week 2020, a joint effort of Infectious Diseases Society of America (IDSA), HIV Medical Association, Pediatric Infectious Diseases Society (PIDS), and the Society for Healthcare Epidemiology of America (SHEA), during an interactive session on Fellows' Day. Copyright Infectious Disease Society of America (IDSA), 2019. Used with permission.
- Citation
- If you refer to this case in a publication, presentation, or teaching resource, we recommend you use the following citation, in addition to citing all specific contributors noted in the case:
Case #20004: Sporotrichoid Rash in an Immunocompromised Patient [Internet]. Partners Infectious Disease Images. Available from: http://www.idimages.org/idreview/case/caseid=586
- Other Resources
-
Healthcare professionals are advised to seek other sources of medical information in addition to this site when making individual patient care decisions, as this site is unable to provide information which can fully address the medical issues of all individuals.
|
|