 |
Chronic neck lesion |
- History of Present Illness
A man in his fifties presented to the Infectious Diseases (ID) clinic with a nodular lesion on the right side of his neck that he had initially noticed about 5 months prior to presentation. The lesion started as an erythematous, painless papule which then became pruritic and gradually increased in size to become nodular in appearance. He was seen by the General Surgery and Dermatology units and underwent an incision and drainage procedure. Cultures sent from this grew Citrobacter koseri and Staphylococcus lugdenensis. He received10 days of Ciprofloxacin followed by 14 days of Amoxicillin/clavulanate. However, these antibiotics did not result in any change of the size or appearance of the lesion. He was then referred to ID clinic for further evaluation.
- Epidemiological History
- He migrated from the Middle East thirty years ago and lives in a large East Coast city in the United States. He travels to the Middle East for about a month annually and the last trip was about 12 months ago. He travelled to Peru about 8 months prior to presentation for an ecotourism trip.
- Physical Examination
Vital signs: Pulse 67 beats per minute, Blood pressure 120/82 mmHg, Temperature 97.8ºF (36.6ºC), Respirations 22 breaths per minute.
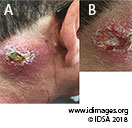
There was a palpable nodular lesion, 5 x 5 cm in size, on the right side of the neck (Fig. 1A). Removal of the overlying eschar revealed a shallow ulcer with granular base (Fig. 1B). Sub-centimeter cervical and sub-mandibular lymph nodes were palpable on the right side. The rest of the general and systemic examination was normal.
 - Figure 1: Neck lesion at presentation (A) and after removal of the eschar (B)

- Studies
Complete blood count was normal including a normal white cell differential. C-reactive protein was normal and liver and renal function tests were normal.
CT scan of his neck showed a soft tissue density on the right side of the neck with thickening of the overlying skin and adjacent fat stranding (Fig. 2). There was no evidence of fluid collection.
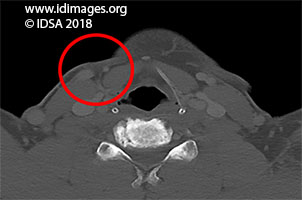 - Figure 2: CT scan of the neck. A soft tissue density is seen in the subcutaneous tissue on the right side of the neck with skin thickening and adjacent fat stranding without evidence of a fluid collection.

- Diagnostic Procedure(s) and Result(s)
He underwent a biopsy of the cutaneous lesion. Histopathology of the biopsy tissue showed dense, pan-dermal granulomas associated with lymphoplasmacytic infiltrate (Fig. 3A). In addition, 2 mm amastigotes were visualized (Figure 3B). The tissue was sent to the New York State Department of Health and Centers for Disease Control and Prevention (CDC). Both facilities carried out polymerase chain reaction tests which identified Leishmania vianna braziliensis as the causative organism.
Bacterial and fungal culture were negative.
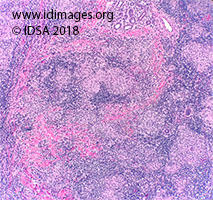 - Figure 3A: Dense lymphoplasmacytic infiltrate is seen with pan-dermal granulomas (40x magnification).

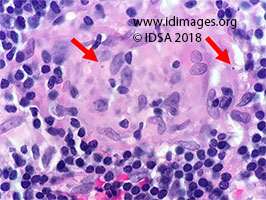 - Figure 3b: Several intracytoplasmic bodies (arrow) are seen measuring around 2 micrometer (400x magnification). These are consistent with amastigotes. Each amastigote has a prominent kinetoplast.

- Treatment and Followup
Given the size of the lesion (5 cm) and the presence of palpable regional lymph nodes, this was considered to be complicated cutaneous leishmaniasis (1). Leishmania vianna braziliensis is associated with development of mucosal leishmaniasis. Our patient denied any symptoms concerning for mucosal involvement and an otorhinolaryngology exam was unrevealing.
Given the size and location of his lesion and risk of mucosal leishmaniasis associated with this species, treatment was initiated with liposomal Amphotericin B: he received 6 doses of 300 mg each on day 1 to 5, and day 10. He was followed closely as an outpatient. The lesion slowly decreased in the size and resolved completely 4-months after completion of therapy (Figure 4)
 - Figure 4: Serial photography of the neck lesion

- Discussion
Cutaneous leishmaniasis is endemic to the Middle East, parts of Central Asia and Latin America, but the species vary in different regions. Leishmania vianna braziliensis is found exclusively in South America including parts of Brazil, Colombia, Peru, Bolivia, Paraguay, Ecuador and Venezuela (2). The sandfly Lutzomyia longipalpis spp. transmits Leishmania vianna braziliensis from forest rodents (reservoir) to humans which are the accidental hosts (1,2).
Being from the Middle East, the patient may have been exposed to Leishmania species endemic to the Old World. The species-specific immunity, however, is not protective against New World species that he likely acquired in Peru.
Leishmania vianna braziliensis is the species most strongly associated with progression to mucosal disease. The risk of mucosal disease persists even after successful treatment and resolution of cutaneous lesions, and mucosal involvement may occur several months after treatment (3).
Pentavalent antimony compounds, sodium stibogluconate and meglumine antimoniate have been administered for the treatment of leishmaniasis for several decades through intravenous, intramuscular and intralesional routes. The exact mechanism of action of these agents is not fully understood, but proposed mechanisms include inhibition of glycolysis and fatty acid metabolism thereby impairing adenosine triphosphate (ATP) formation within infected macrophages, direct inhibition of Leishmania purine synthesis, and enhanced parasite killing via induction of nitric oxide synthesis and reactive oxygen species generation. While these continue to be first line agents for the treatment of Leishmaniasis in several parts of the world, systemic administration is associated with significant adverse events including severe arthralgias, myalgias and cardiotoxicity which often leads to interruption of treatment. Moreover, there have been increasing reports of resistance to treatment in several species. In particular, failure rates of up to 45% have been described in vianna braziliensis species.
In a small clinical treatment trial of Leishmania vianna braziliensis, liposomal Amphotericin B resulted in complete cure in 85% and partial response in 11%. In contrast, treatment with sodium stibogluconate resulted in 29% treatment failure and significantly higher adverse effects (1,4). We therefore chose liposomal Amphotericin B for our patient. It was administered in six doses of 300 mg per dose on day 1 through 5 and on day 10 as per recommendations from the Infectious Diseases Society of America. The erythema and inflammation around the lesion increased slightly during the initial 10 to 14 days post-treatment, a paroxysmal worsening which is anticipated as the parasites are killed. Thereafter the lesion slowly improved and almost completely healed by 4 months after completion of treatment.
- Final Diagnosis
Complicated cutaneous new world Leishmaniasis with Leishmania viannia braziliensis
- References
-
- Aronson N, Herwaldt BL, Libman M, Pearson R, Lopez-Velez R, Weina P, Carvalho EM, Ephros M, Jeronimo S, Magill A. Diagnosis and Treatment of Leishmaniasis: Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH). Clin Infect Dis. 2016 Dec 15;63(12):e202-e264
PMID:27941143 (PubMed abstract)
- Magill AJ. Cutaneous leishmaniasis in the returning traveler.Infect Dis Clin North Am. 2005 Mar;19(1):241-66, x-xi
PMID:23529965 (PubMed abstract)
- Machado-Coelho GL, Caiaffa WT, Genaro O, Magalhães PA, Mayrink W. Risk factors for mucosal manifestation of American cutaneous leishmaniasis. Trans R Soc Trop Med Hyg. 2005 Jan;99(1):55-61.
PMID:15550262 (PubMed abstract)
- Solomon M, Pavlotzky F, Barzilai A, Schwartz E. Liposomal amphotericin B in comparison to sodium stibogluconate for Leishmania braziliensis cutaneous leishmaniasis in travelers. J Am Acad Dermatol. 2013 Feb;68(2):284-9
PMID:22858005 (PubMed abstract)
- Notes
ID week Fellows' Day 2018 - oral presentation
This case was contributed by:
Fatima Adhi, MD (1); Gabriel Rebick, MD (2) and Ellie Carmody, MD, MPH (2).
(1) Respiratory Institute, Cleveland Clinic Foundation, Cleveland, Ohio, USA
(2) Division of Infectious Diseases and Immunology, New York University School of Medicine, New York, NY, USA
The case was originally presented at ID Week 2018, a joint effort of Infectious Diseases Society of America (IDSA), HIV Medical Association, Pediatric Infectious Diseases Society (PIDS), and the Society for Healthcare Epidemiology of America (SHEA), during an interactive session on Fellows' Day. Copyright Infectious Disease Society of America (IDSA), 2018. Used with permission.
Last reviewed: 9 March 2019
- Citation
- If you refer to this case in a publication, presentation, or teaching resource, we recommend you use the following citation, in addition to citing all specific contributors noted in the case:
Case #18012: Chronic neck lesion [Internet]. Partners Infectious Disease Images. Available from: http://www.idimages.org/idreview/case/caseid=568
- Other Resources
-
Healthcare professionals are advised to seek other sources of medical information in addition to this site when making individual patient care decisions, as this site is unable to provide information which can fully address the medical issues of all individuals.
|
|